A new drug could stop death before it starts – but at a cost
As hay fever season approaches, once again, for allergy and asthma sufferers in the northern hemisphere, researchers in California are working on a new treatment that could completely prevent childhood asthma — in a way that works less of the bacteria in the gut.
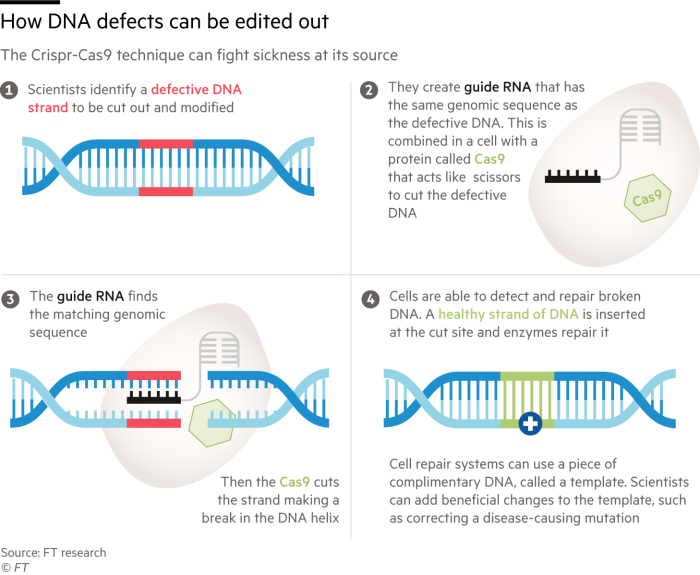
Scientists at the universities of Berkeley and San Francisco found a link between these viruses and the chances of childhood asthma. So, now, using Crispr gene editing – a new technology that allows correct changes to be made in DNA – they are exploring how to change bacteria to remove the risk of children developing lung conditions.
Susan Lynch, head of San Francisco’s Benioff Center for Microbiome Medicine and principal investigator of the San Francisco: asthma project.
This is one of the few advances in technology and medicine that can prevent diseases before they start – helping to save a long time to provide health care and avoid suffering for patients.
And these preventive treatments are becoming even more important, as health systems strain under the burden of an aging population and increasing levels of chronic diseases.

Lynch first identified a small molecule in the gut bacteria of infants that was linked to the risk of childhood allergies and asthma back in 2019. This led to a project to remove the bacteria’s ability to make the molecule. ‘pull, rather than remove the bacteria itself,’ explains Lynch. “It’s precision engineering as opposed to haphazard extraction,” he says.
A treatment like this comes with huge research and development costs, but, by preventing chronic diseases, it can lead to long-term savings: the annual cost of asthma in the US alone is $56bn, a lot -related to hospital stays, according to the Asthma and Allergy Foundation of America.
In addition, treating common diseases such as asthma by modifying genes may help reduce resistance to viruses associated with asthma that are more common in people with asthma, Lynch adds.
The project will use tools developed by the Innovative Genomics Institute, founded by Nobel Prize-winning scientist Jennifer Doudna who was one of the discoverers of the ability to sequence DNA Crispr- Cas9.
Although Lynch’s work is related to asthma, the Center is exploring how to use Crispr in other difficult disease areas. Brad Ringeisen, chief executive officer of the IGI, identified links between inflammatory bowel disease and Alzheimer’s disease.
“Wouldn’t it be great if you could turn off those processes, or remove the microbiome from the beginning where you’re already preventing those diseases, or push them forward in life, instead of trying to cure something that is really recalcitrant?” says Ringeisen.
But the technology is still in its infancy and widespread adoption won’t happen for many years. There are also significant upfront costs to gene editing treatments that may outweigh the cost savings later. The only approved Crispr-based therapy to date, Vertex Pharmaceuticals’ Casgevy, which can treat sickle cell disease, is complex to administer and costs $2.2mn per treatment.
Cost is also a point of contention for new weight-loss drugs known as GLP-1s, which can treat obesity and diabetes, as well as reduce the risk of heart disease and liver problems, to follow clinical trial data.
One of the drugs, Novo Nordisk’s Wegovy, received approval in the US for the prevention of heart disease and other cardiovascular events in March. But the drug has faced political criticism for its cost, with Senator Bernie Sanders saying Wegovy’s list price of $1,349 a month is “too high”.
David Wheeler, professor of kidney medicine at the University of London, says that the high costs should be assessed against the growing problem of chronic diseases. Rates of advanced chronic kidney disease (CKD), for example, are expected to rise 60 percent by 2032 in eight countries, including the US, China and Brazil, according to a study by scientists at UCL and drug maker AstraZeneca.
The findings are of clear interest to AstraZeneca: Its drug Forxiga developed for diabetes and heart failure has also shown success in preventing severe CKD. It sold nearly $2bn in the first few months of 2024, making it the company’s best-selling drug.
However, potential customers need to be convinced of the value of anti-inflammatory drugs, as generic drugs can often be very expensive. For extended public health budgets, public health investments may be better value for money.
Fairly funded public health schemes are a good example, says Dave Buck, senior fellow on public health and inequality at the King’s Fund, a British health think tank.
In the UK, the most effective prevention measures have been local authority schemes for smoking cessation and promoting healthy eating. These are supported by public health grants from the local government, which are 3-4 times cheaper than the use of the national health service, which supports the majority of treatment in the country, according to the study of 2020 by academics at the University of York.
But, while NHS funding has been largely protected in recent years, real per capita spending on public health grants has fallen by 28 per cent since 2015/16, the Health Foundation get it.
“Obviously I’m not against high-tech stuff but you need to get the basics right,” says Buck. “You need to keep pushing the boundaries but also focus on what’s behind.”
#drug #stop #death #starts #cost